Dental Public Health
Dental Public Health (DPH) is the science and art of preventing oral diseases, promoting oral health, and improving the quality of life through the organised efforts of society.
Specialist training in DPH usually starts with a master’s degree in Dental Public Health or Public Health with a significant oral health component.
Individuals who already have one of these qualifications before entering specialist training, will normally only be required to undertake a further three years of specialist training. MPH courses must be approved by the Specialist Advisory Committee in Dental Public Health.
In Yorkshire and the Humber, DPH trainees are employed by NHS Trusts or Universities and their service work is based on honorary appointment with NHS England. This allows opportunities for placements with NHS Integrated Care Boards (ICBs), local authorities, and other organisations as required.
Specialist trainee are required to be successful in the Intercollegiate Specialty Fellowship Examination (ISFE) before completion of the programme as a summative assessment. Once NHS England WTE is satisfied that the trainee has satisfactorily completed all necessary assessments, including the ISFE exit examination, they will forward a recommendation for award of the Certificate of Completion of Specialist Training to the General Dental Council.
Once appointed as consultant, you are expected to:
- Provide specialist dental public health advice and support to the NHS England, local authorities, ICBs, other partners and the public.
- Provide specialist dental public health advice and support and professional leadership to advocate for oral health improvement, reducing inequalities, and improvements in oral health services by developing and supporting the implementation of oral health strategies.
- Support the development of the dental public health workforce including being responsible for their own personal development and demonstrating strategic leadership and development of dental and other health professionals with regard to dental public health.
- Participate and where appropriate, lead on areas of national or regional work related to the Oral Health national agenda working in collaboration with other Consultants in Dental Public Health, the NHS England national dental team, the Office of the Chief Dental Officer, regional Healthcare Public health teams and the Office for Health Inequalities and Disparities (OHID).
"We are a small specialty and work very closely as a team to deliver a high quality specialty training programme in dental public health. Trainees have the opportunity to train in urban and rural locations hosted within health and social care organisations and the university.
Training Programme Directors
Dr Sandra Whiston
In post until end of December 2023.
Further information on recruitment, ARCP, study leave and period of grace can be found here.
Trainees in dental public health must undertake 12 months of academic training at master’s level or equivalent, for example: an MSc in Dental Public Health or Master of Public Health (MPH), which includes specific dental modules. This will involve training in research skills and potentially a poster or journal publication.
There are a few academic posts in universities. Academic dental public health posts funded jointly by the universities and NHS are sometimes available.
Higher specialist training programmes in Dental Public Health normally require four years’ study. Trainees will be expected to complete three years of NHS training and one year of formal academic training at master’s level or equivalent.
The purpose of the training programme is to give trainees supervised experience in the theory and practice of Dental Public Health and the opportunity to develop the knowledge, skills, attitudes, and overall competence required by a consultant in the specialty.
Formal Academic Training
Trainees must undertake 12 months of academic training at master’s level or equivalent, for example: an MSc in Dental Public Health or Master of Public Health (MPH), which includes specific dental modules.
Individuals with these academic qualifications, who enter the specialist registrar grade, will normally only be required to undertake a further three years of specialist training.
MPH courses must be approved by the Specialist Advisory Committee in Dental Public Health and the Examination Board for the Diploma in Dental Public Health (DDPH) as being adequate to enable individuals to sit the DDPH Examination (although they will not be required to do so).
Completion of Training
Trainees must pass the Intercollegiate Speciality Fellowship Examination on completion of the training programme and achievement of satisfactory structured assessments. Trainees can then be recommended for the award of a Certificate of Completion of Specialist Training in Dental Public Health (CCST).
You may start working as a locum or acting consultant before a substantive post is available. The person specification is available at:
http://www.rcseng.ac.uk/fds/faculty-advisors/appointment-procedures/docs/PS%20-%20DPH.pdf/view
There are a few academic posts in universities. Posts funded jointly by the universities and NHS are sometimes available.
To be appointed as a Senior Lecturer, you are expected to have substantial publications and a record of obtaining research funding, as well as being a fellow of the Higher Education Academy. Please click here for further details: http://www.heacademy.ac.uk/ProfessionalRecognition.htm.
Consultants in Dental Public Health sometimes also hold honorary academic or research posts in universities. These posts can include: honorary teacher, lecturer, senior lecturer, senior research fellow or honorary research fellow.
After obtaining your CCST in Dental Public Health, you can also become a Fellow of the Faculty of Public Health without examination. Please click here for details http://www.fph.org.uk/exams/exemption/fellowship_exemption.asp#PHdentists.
Some of you may be interested in becoming a Director/Deputy Director of Public Health. Further information on senior public health appointments is available athttp://www.fph.org.uk/prof_affairs/guidance_for_public_health_appointments/default.asp.
There is no formal on-call, except for those involved in Health Protection. However, out of hours working is required occasionally, for example, evening meetings.
_____________________________
The Intercollegiate Surgical Curriculum Programme Website
This site houses the curriculum for the dental specialties and, in a secure area, trainees’ electronic portfolios and the learning agreements which support training.
All trainees will eventually use the e-portfolio but this will be done on a rolling programme by specialty. Consultants and other professionals who will be training, assessing and supervising training will also need to register.
Useful Links
- British Society of
Community Dentistry (BASCD)
http://www.bascd.org
Dental Public Health Specialty Training in Yorkshire and the Humber
Do you like innovation? Do you hate monotony? Would you like to lead on projects that could improve the life of entire communities? If your answer is yes, then I invite you to apply for dental public health specialty training in Yorkshire and the Humber.
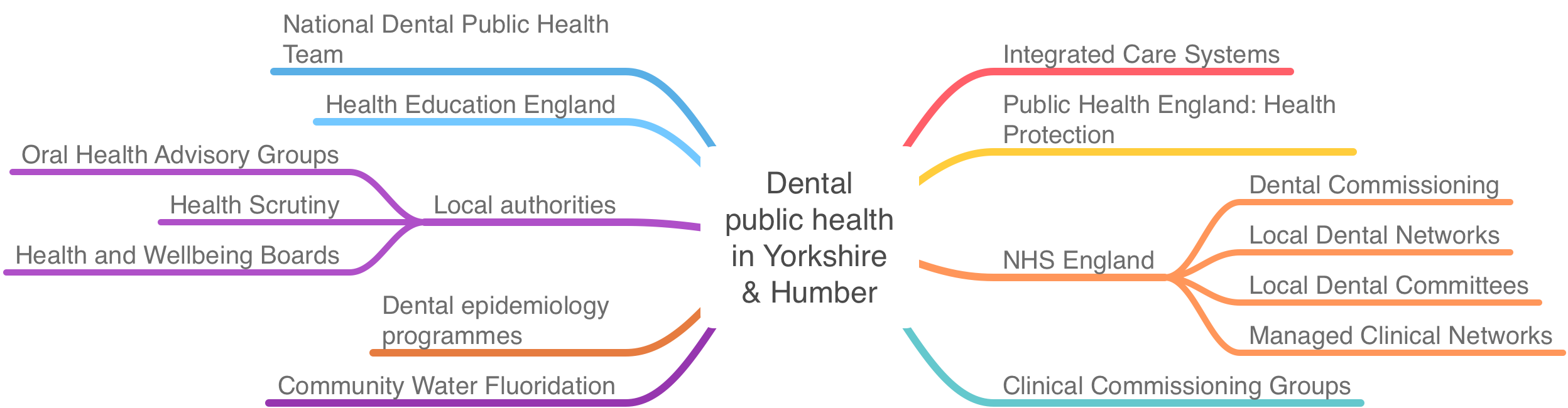
When I decided to train in Yorkshire, I made my decision based on three factors: the type of work that I would be doing, the people who I would be working with and the location where I would be living. And to a certain degree some of these factors are linked to each other. Our region is famous for the innovative work that is taking place both in terms of clinical service as well as academic research. This work is facilitated by the strong partnerships between key stakeholders like Public Health England, NHS England, Health Education England, local authorities, The University of Leeds, and others. Yorkshire is a huge geographical area that has both large and busy cities as well as vast rural and coastal areas with charming towns and villages. You get to experience different ways of working in different areas and identify creative solutions to improve oral health and reduce inequalities within these populations. Although there is no patient contact in dental public health, your work has an impact at populational level.
In my first year of training, I had the opportunity to support four local authorities and get first-hand experience of working with the councils by being embedded within the local public health teams. We worked on oral health needs assessments and strategies, I supported oral health promotion services and oral health advisory groups and presented in front of locally elected members on Health Scrutiny and Health and Wellbeing Boards.[1] Most of this work did not end in the first year but it carried on throughout the training by continuing to provide support and specialist advice to the councils for developing new service specifications for oral health promotion and helping to implement their strategies and action plans.
There are no two identical days in my training. You can choose from a variety of project opportunities to meet the competencies required for completion of training. A large part of my work is supporting NHS England and NHS Improvement dental commissioning team. Yorkshire and the Humber was one of the first regions in the country to develop a flexible (transformational) commissioning programme that allows dental care providers to remove some of the pressures of the UDA system and deliver more preventative work through skill mix.[2] Some of this work has been targeted to improve access for certain groups like homeless and other socially marginalised groups.[3]
Using the principles of system leadership, I had the opportunity to work with a variety of organisations to develop a regional public health placement for Foundation Dentists (FD). For the first time ever, foundation dentists were helping the COVID-19 pandemic response by vaccinating people against flu and against COVID-19.[4]
And this brings me to my research. As an academic trainee, my main research interest is on the association between oral and general health and on reducing the interprofessional barriers between dentistry and medicine.[5] This is also one of Leeds Dental School’s strategic research objectives. The School initiated the PROSPECT initiative on oral-systemic research. Furthermore, the periodontal research group has strong links with one of the largest rheumatology research groups in the country, also hosted by The University of Leeds.
If these examples sound appealing, I assure you, this is just a small selection of the opportunities that I had the chance to work on during my specialty training. There are many more exciting opportunities waiting for you in Yorkshire. What are you waiting for?
Designed by S Serban, Dental Public Health Trainee, 2021
[1] The Yorkshire Post, Council to explore possibility of fluoridation of water to improve dental health of children
[2] Mustufvi Z, Barraclough O, Hearnshaw S, Whiston S, Grant S, Serban S, et al. Flexible Commissioning: A prevention and access focused approach in Yorkshire and the Humber. BDJ In Practice. 2020;33(2):20-2.
[3] Csikar J, Vinall-Collier K, Richemond J, Talbot J, Serban S, Douglas G. Identifying the barriers and facilitators for homeless people to achieve good oral health. Community dental health. 2019;36(2):137-42.
[4] Serban S, Mustufvi Z, Kang J, Simon SE, Grant S, Douglas G. The Dental Team: An Additional Resource for Delivering Vaccinations (vol 7, 606242, 2020). FRONTIERS IN MEDICINE. 2021;8.
[5] Watt RG, Serban S. Multimorbidity: a challenge and opportunity for the dental profession. British Dental Journal. 2020;229(5):282-6.
To confirm Dental Public Health Registrars on NHSE placements are currently not covered under the standard NHSE Crown Indemnity contract.
All Dental Public Health Registrars are GDC Registrants and all are expected to have appropriate indemnity cover, as required for registration with the GDC. This could be provided through personal cover*, or the Dental Public Health Registrar can explore two of the following options to ensure they have appropriate indemnity cover. The registrar would need to discuss this with their lead employer and ES to ensure an agreed process.
- The registrar will pay, annually, for the cover and claim it back through their expenses system with their lead employer.
- The lead employer will pay for the cover annually subject to a local agreement with NHSE
Any reimbursement to the individual will need to be supported with a detailed receipt or invoice from their chosen Medical Defence Organisation.
*Please note NHS England will not reimburse costs for any personal indemnity taken out with a Medical Defence Organisation; Dental Public Health registrars are only able to claim indemnity costs as part of their placement and for work they need to cover as part of their training programme for NHS England.
If you encounter any further problems please contact the Office of Public Health Professional Functions at - england.nhse-ph-professionalappraisals@nhs.net